by Angelica Lo Duca, Clara Bacciu, Andrea Marchetti (IIT-CNR)
The use of distributed ledgers (DL) in healthcare applications presents the opportunity to create new interoperable and secure environments, from which both medical professionals and patients can benefit.
Within the Institute of Informatics and Telematics of the National Research Council in Pisa, a new working group on distributed ledgers (DL) is being set up. The main objective of the group is to study DL technology and implement DL-based solutions for different scenarios, such as traceability of products and health care applications (HCAs). In this paper we focus on HCAs and we illustrate how they can be transformed with the introduction of DL.
For many years, electronic health records (EHRs) about patients’ health care have been stored in different HCAs, which essentially are very heterogeneous and are not designed to manage multi-institutional and lifetime medical records (Figure 1). In fact, different health institutions do not usually share a common HCA, and EHRs associated to the same patient and stored by different institutions do not refer each other. This means that it is not possible to extract a patient’s history simply from their EHR. In some cases, even within the same institution, two EHR associated to the same patient are not connected. Thus, a patient moving from one institution to another, must register each time to the local HCA, provided by the current institution, in order to build his/her local EHR. In addition, the patient should provide the current institution with the previous resignation sheet, which contains all the information related to the patient’s previous recovery. This process, which often is tedious, could also introduce errors and lose potentially useful information about the patient. As a consequence, medical professionals may end up working with incomplete information.
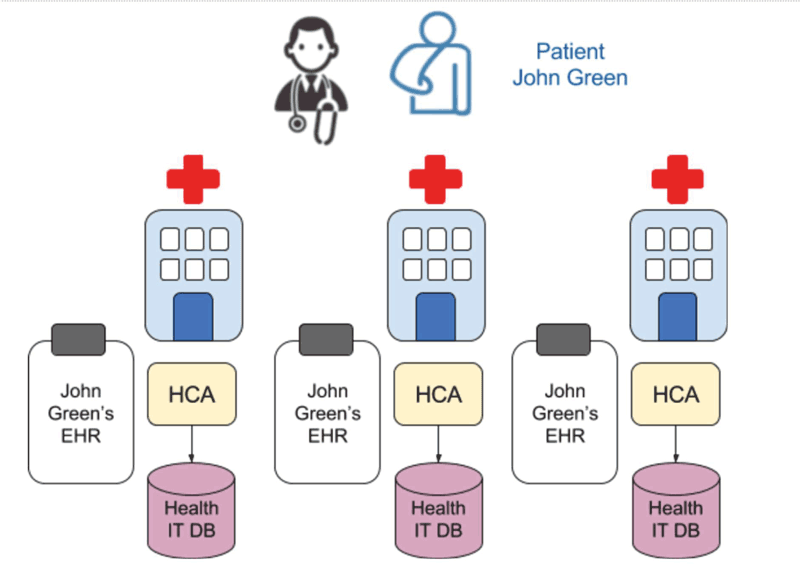
Figure 1: Traditional management of EHRs.
DL can potentially transform HCAs as they provide new opportunities for health IT systems, by guaranteeing interoperability among heterogeneous applications in a secure way [1]. In fact, an architecture based on DL does not require node homogeneity: the only requirement is that a node of the system can be identified in a secure way, i.e., it is equipped with a pair public/private key. Security provided by DL through authentication, confidentiality and accountability, allows patients’ information to be protected from unauthorised access. Both doctors and patients could benefit from the use of DL in HCAs: on the one hand, doctors could access more information about a patient, such as their health history, laboratory results, prescribed medications, and even information extracted from personal bio sensors. On the other hand, it would also allow patients to access their full EHR, anywhere and anytime and it would remove the need for individuals to register to a new HCA for each hospitalisation. Furthmore, the whole health sector may benefit from the adoption of DL, through economic savings and increased efficiency of the health IT system.
A variety of companies have already entered the ecosystem, trying to capitalise on opportunities created by DL applied to HCAs [2, L1, L2, L3]. All the existing models in this field separate databases where all EHRs are stored from the database which specifies how to access the data, i.e., the DL [3]. Figure 2 illustrates how DLs can be used in HCAs: a data lake is used to store all the patients’ information (laboratory results, doctors’ prescriptions and so on). The DL is exploited to store all the pointers to the data lake in a secure way. Patients and providers (e.g., institutions, doctors, laboratories) are equipped with public/private keys, which allow them to authenticate each other. Patients can give partial and time-limited view of their EHRs to one or more providers through access control policies, regulated, for example, by means of smart contracts. Once the medical exam is ready, the provider signs it with a digital signature and sends it back to the client. If the client accepts it, the exam is added to the DL.
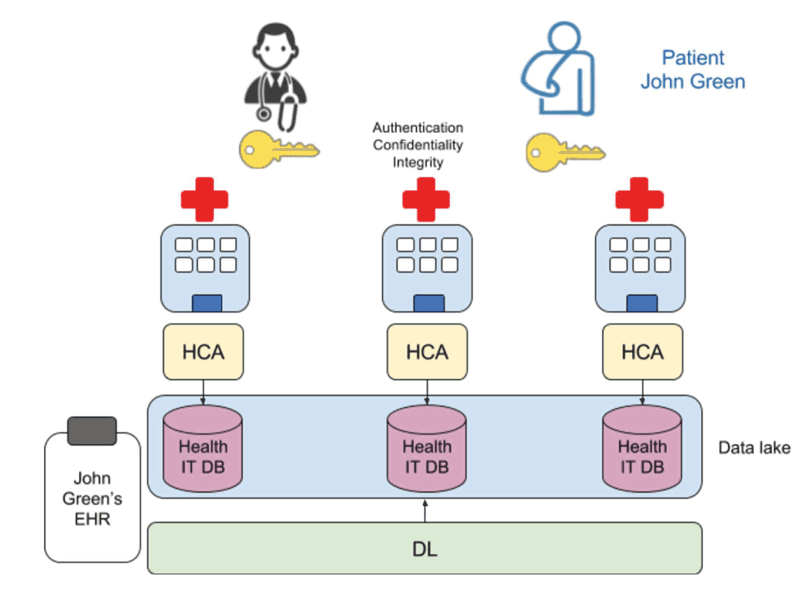
Figure 2: How the use of DL can transform the management of EHRs.
DLs undoubtedly represent a real opportunity for HCAs because they do not require any changes to the existing health IT databases, which are still maintained separated. Only a new database, i.e., the DL, should be added to the network, containing only the pointers to the original health IT databases. The DL would play two roles: to connect all the existing health IT databases and to guarantee privacy and integrity of EHRs.
Links:
[L1] https://deepmind.com/applied/deepmind-health/
[L2] https://gem.co/health/
[L3] https://blockchainhealth.co
References:
[1] M. Mettler: “Blockchain technology in healthcare: The revolution starts here”, in e-Health Networking, Applications and Services, Healthcom 2016, pp. 1-3, IEEE, 2016.
[2] A. Ekblaw et al.: “A Case Study for Blockchain in Healthcare: ‘MedRec’ prototype for electronic health records and medical research data”, Whitepaper, 2016.
http://dci.mit.edu/assets/papers/eckblaw.pdf
[3] L. A. Linn, M. B. KOO: “Blockchain for Health Data and Its Potential Use in Health IT and Health Care Related Research”
https://www.healthit.gov/sites/default/files/11-74-ablockchainforhealthcare.pdf
Please contact:
Andrea Marchetti, IIT-CNR, Italy
+39 050 315 2649