by Ioannis Tollis and Nicholas Ayache
Initiated by the European Commission as a major multidisciplinary scientific challenge, the Virtual Physiological Human (VPH) aims to develop robust, in silico models of human physiology and pathology. The desired outcomes include the identification of novel diagnostic biomarkers, the optimization of clinical decision-making and the discovery of innovative therapies. In this way, individualized models of human function could serve as virtual testbeds for a better understanding of pathophysiological processes (ie the disturbance of normal mechanical, physical and biochemical functions), as well as evaluating potential therapeutical strategies in silico.
This scientific direction is reflected in the recent calls for projects for the European Union's 7th Framework Programme on VPH, which will target:
-
patient-specific computational modelling and simulation of organs or systems targeting specific clinical needs such as prediction of diseases
-
data integration and knowledge extraction, and most importantly
-
clinical applications and demonstration of the tangible benefits of patient-specific computational models.
This European initiative will give rise to new environments for predictive, individualized, evidence-based, more effective and safer healthcare. In addition, better therapy and the modelling of adverse drug effects will reduce medical errors and improve patient safety.
However, in developing such patient-specific models it is crucial to implement multi-layered models that describe different properties (eg electrical, mechanical and biochemical), and appropriate image analysis and data assimilation tools to identify their specific parameters from patient images. An ultimate goal is to meaningfully integrate these models to describe/model/mimic some life function, rather than individual properties, at different scales; for example, from cellular dynamics to organ function. To realize this ambitious scientific vision it will be necessary to address a number of challenges related both to infrastructure and data management, computational issues, validation and legal ethical issues.
A new ERCIM Working Group for Pathophysiology Modelling
In order to contribute to the European effort on the Virtual Physiological Human a new ERCIM Working Group (WG) on the Digital Patient was created. This WG facilitates multidisciplinary research in this domain, with a special emphasis on:
- computational frameworks for modelling and simulation of pathophysiological human function at multiple levels (from molecular/genetic to tissue/organ)
- multiparameter and multilevel data and information visualization, as well as tools and novel interaction paradigms relevant for this domain (eg for mixed reality such as tumour growth simulation in real 3D patient data), and user interfaces for specific medical applications (eg educational GUIs for training in 3D simulations)
- the image analysis and data assimilation issues related to coupling/fusion of anatomical models with imaging data of tissue properties (eg X-rays, US, CT, MRI, PET, SPECT, optical imaging etc).
The ERCIM WG on the Digital Patient intends to promote interaction between the relevant ERCIM R&D groups, and to facilitate cross-fertilization and synergistic activities in collaboration with other groups and initiatives such as the Europhysiome initiative currently funded by the European Commission.
To date, many ERCIM (and non-ERCIM) members have joined this effort. The last WG meeting was held in Nice in October 2006, and identified three interesting research directions:
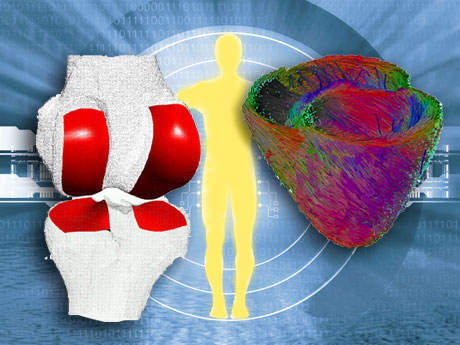
1) Cardiovascular Modelling
Cardiovascular modelling is important for the therapy planning and guidance of cardiovascular therapies. An example is Atrial and Ventricular Radio-Frequency ablation for the surgical treatment of atrial/ventricular flutters or fibrillations. The therapy consists of burning cardiac cells that are causing pathological electrical pathways. Prior to burning the cardiac tissue, the cardiologist must precisely locate the pathological cardiac cells by reading electrical signals measured by more than ten electrodes inserted through an endovascular procedure. The real-time interpretation of those signals requires significant training, and the planning and execution of the therapy could be made more efficient with the use of electrophysiological models.
Another important example is Cardiac Resynchronization Therapy. Resynchronization therapy artificially stimulates the myocardium through implanted electrodes in order to limit the ventricular dysfunction caused by asynchronous ventricular contraction. Although a number of cardiac resynchronization therapeutic strategies exist (regarding the selection of the number, location and delay between those electrodes), nearly 30% show no real improvement in cardiac function. It is therefore plausible that a thorough planning of CRT based on a personalized cardiac model could greatly assist the cardiologist in deciding the optimal strategy.
2) Musculoskeletal Modelling
Musculoskeletal modelling aims to predict musculoskeletal behaviour (eg bone kinematics, tissue deformation, tissue degeneration and tissue reconstruction) from the morphology, kinematical constraints, mechanical constraints or neuromuscular impulses. In addition to applications in orthopaedics (eg early detection of osteoarthritis, prosthesis design, osteotomy planning, tendon lengthening and ligament reconstruction), this would be of use in kinesiology for movement optimization (eg reduction of tennis elbow), rehabilitation and ergonomics (eg minimization of physical fatigue under specific constraints). From the physiological point of view, a link between large-scale studies (anatomy-based virtual humans animated from motion capture and EMG) and small-scale studies (deformation analysis due to local fibre actuation) has not yet been achieved. Bridging those domains through computationally efficient and scalable mechanical simulation methods is a major challenge.
3) Oncology Modelling
Oncology modelling focuses on the simulation of tumour growth and/or the response of tumours and physiological tissues to different therapeutic regimes (eg chemotherapy, radiotherapy or combined therapy). In this way, the optimal therapy decision for individual patients can be selected on the basis of the best simulated therapy outcome. For this to be successful, it is crucial to test these models against reality and thus assess their usefulness in clinical practice. From a purely technical perspective, the challenges include: the development/refinement of a number of hybrid discrete Monte Carlo/cellular automata and continuous differential equation simulation models of normal tumour growth and response to therapeutic modalities; image analysis tools such as geometrical normalization (eg 3D MRI before and after therapy); extraction of relevant information (eg accurate tumour delineation also considering liquefaction during therapy); normalization and quantification from images (eg differential gene expression, tissue density); and visualization. The main clinical applications are glioma and nephroblastoma (Wilms tumour). These applications have been selected on the basis of existing work, experience and ongoing clinical collaborations in relevant projects. The ultimate goal is to optimize the therapeutic strategy by conducting, in a patient-specific setting, in silico experiments on tumour growth and tumour and normal tissue response to therapeutic schemes.
This wide range of research interests was the inspiration behind the proposal for a special theme on the Digital Patient for ERCIM News. This issue features articles addressing either European projects or specific scientific achievements related to the VPH. A number of articles deal with applications of 'Pathophysiology modelling' (at the organ level), mainly in the three areas previously described. However, in order to build multidimensional models of the human function, it is essential to extract information from all possible scales. This is addressed by articles on the subtopic 'Data analysis and imaging' in this special theme. Several articles address 'System biology modelling', since modelling at smaller scales (cellular and even molecular) is an essential part of a 'holistic' VPH. Lastly, the article by Vincent Duffy deals with Digital Human Modelling for perception-based safety design.
Links:
White Paper on the Virtual Physiological Human:
http://europa.eu.int/information_society/activities/health/
docs/events/barcelona2005/ec-vph-white-paper2005nov.pdf
ERCIM Digital Patient Working Group: http://www.ercim.org/wg/Digital_Patient/
Europhysiome initiative: http://www.europhysiome.org
Please contact:
Ioannis Tollis
ICS-FORTH, Greece
E-mail: tollis![]() ics.forth.gr
ics.forth.gr
Nicholas Ayache
INRIA, France
E-mail: nicholas.ayache![]() inria.fr
inria.fr