by Mohamed Boukhebouze, Stéphane Mouton and Jimmy Nsenga
A personal on-board data-mining framework that relies on wearable devices and supports on-board data stream mining can help with disease prediction, risk prevention, personalized intervention and patient participation in healthcare. Such an architecture, which allows continuous monitoring and real-time decision-making, can help people living with diseases such as epilepsy.
The emergence of systems biology, big data tools and wearable computers is transforming medicine from a reactive paradigm that focuses on treating disease, to “P4 medicine” that focuses on predicting diseases, preventing the risks of developing diseases, personalizing interventions based on the patient context and participation of the patients in the management of their own health [1]. This new paradigm pledges to improve healthcare through early detection of disease and helping patients to make decisions about prevention and treatment.
For the P4 medicine approach to be successful, personal (patient-specific) data should be collected and mined at a large scale in order to discover hidden patterns and make effective decisions. The wearable devices can perform ubiquitous collections of a large subset of personal data and be used as interface to data mining algorithms. The latter are executed remotely on cloud-based infrastructure that provides high performance processing resources [2]. However, for P4 medicine to fully accomplish its goals, wearable devices must also execute offline data stream mining. Indeed, the on-board data mining execution allows continuous monitoring and real-time processing, which can help with early disease detection and prevention. Therefore, on-board execution could improve the mobility and safety of patients and enhance their quality of life.
Despite the great progress in wearable technology and ubiquitous computing, many issues must be addressed in order to implement efficient on-board data mining for P4 medicine, including:
- Resource limitation. Wearable devices are limited in terms of computational power, energy consumption, storage and memory capacity and bandwidth.
- Context and resource changes. Ubiquitous data stream mining has to deal with patient situation changes and device disconnection.
- Data quality. Despite accrued sophistication of current sensors, accuracy of gathered data is not always ensured. Furthermore, variable data rates can cause problems [2].
To deal with these issues, we propose an on-board personal data-mining framework for P4 medicine, currently under development in our research centre, relying on a network of wearable devices to monitor the patient in real-time based on P4 medicine principles:
- Predicting the risk of developing diseases or faintness (e.g., epilepsy seizure, heart attack) based on well-defined patterns. The framework notifies patient once a risk is identified.
- Preventing certain diseases or faintness by providing recommendations that help to avoid or reduce the risk of developing them.
- Personalizing the prediction and prevention recommendations by taking into account the context of patients (profile, medical history, actual environment, etc.).
- Participation of the patients in the learning and refinement of the prediction and prevention models by providing feedback about issued notification and recommendations.
The proposed framework deals with the on-board processing issues by combining three approaches (see Figure 1):
- A distributed data mining approach is used to execute data mining algorithms concurrently over the network of wearable devices. This approach helps to address the computational constraints and energy efficiency issues by distributing data processing across devices.
- A context-aware and resource-aware adaptation strategy is used to detect changes of patient situation or devices and automatically adjust the parameters of data mining algorithms. This approach is also used to dynamically distribute the load of data mining algorithms based on resource availability.
- A probabilistic data mining approach is used to deal with data quality issues by computing data variation and uncertainty. In this way, risk prediction and prevention recommendations should be improved because the full range of possible outcomes can be taken into account.
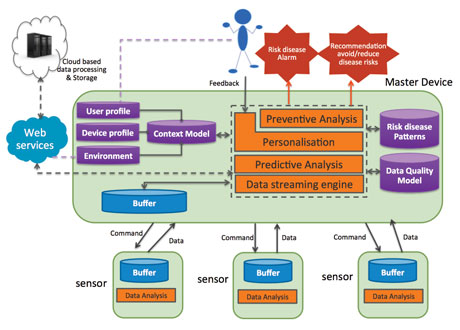
Figure 1: An architecture overview of the device part of the Framework for P4 Medicine.
To validate our proposed framework, we are considering epilepsy as a case study – in particular, refractory epilepsy patients who do not respond to conventional treatment. Thirty percent of people with epilepsy have refractory epilepsy, [3] a very debilitating form of the disease since the seizures are random and not controllable with medication. The proposed on-board data-mining framework can be used to continuously monitor refractory epilepsy patients and notify them of seizure risks based on early detection patterns that are developed by our academic partner LISA Laboratory – Université Libre de Bruxelles. These notifications contribute to improve the safety and quality of life of individuals affected by refractory epilepsy. Furthermore, the framework can provide context-aware recommendations to reduce seizure risk by analysing the triggering factors (e.g., stress level), consequently helping to reduce seizure frequency. Finally, the collected data could be used by epilepsy specialists to better identify appropriate treatment.
Links:
P4 Medicine Institute: http://www.p4mi.org
LISA Laboratory: lisa.ulb.ac.be
References:
[1] L. Hood and S. H. Friend: “Predictive, personalized, preventive, participatory (P4) cancer medicine,” Nature Reviews Clinical Oncology, vol. 8, no. 3, pp. 184–187, 2011.
[2] M.M. Gaber, J.B. Gomes, and F. Stahl: “Pocket data mining”. Springer Book, 2014, ISBN: 9783319027111, pp. 1–112.
[3] P. Kwan, and M.J. Brodie: “Early identification of refractory epilepsy.” New England Journal of Medicine, 2000, 342(5), 314-319.
Please contact:
Mohamed Boukhebouze,
CETIC, Belgium